BME100 s2017:Group4 W1030AM L1
| Home People Lab Write-Up 1 | Lab Write-Up 2 | Lab Write-Up 3 Lab Write-Up 4 | Lab Write-Up 5 | Lab Write-Up 6 Course Logistics For Instructors Photos Wiki Editing Help | |||||||
OUR TEAM
LAB 1 WRITE-UPHealth Care Issue
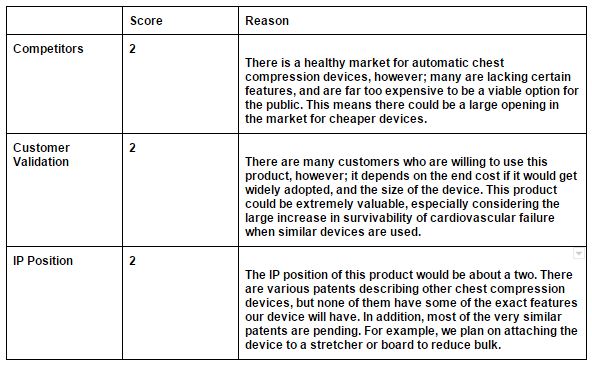
A need of an efficient way for EMS crews to manage resuscitating an unconscious patient with CPR so that they can attend to the patient’s other medical needs. The proposed device will primarily be used in treating people who are not breathing due to a heart attack, stroke, or ingestion of liquids. Currently, the cost of automatic chest compression devices or ACCDs out on the market ranges around $13,000-$15,000(1). The high cost of ACCDs makes it so that most ambulances and hospitals are not equipped with one. Furthermore, the quality of chest compressions provided even by trained EMS technicians can be inconsistent(2) and experience multiple interruptions as the crew scrambles to deal with other issues. The proposed device is an adjustable (such that it can be effective on people of different masses and heights), water-resistant and cheaper ACCD which can be attached to a stretcher and most other stable surfaces.
1. Medical Device Depot. http://www.medicalexpo.com/medical-manufacturer/chest-compressor-1187.html.
Customer Validation
2.Fred Durham (Assistant fire marshal of Arizona) - http://www.dfbls.az.gov/contacts/OFMInspectors.aspx 3.Anita Chambers (Odulair, Mobile Clinics CEO) http://www.odulair.com/management.html 4.Michael Synder (Patient) http://www.emsworld.com/article/12121129/the-evidence-for-automated-chest-compression-devices 5. Robert L. Meyer(CEO Phoenix Children’s hospital) http://www.phoenixchildrens.org/about/executive-bios#steven-spalding 6. Toni Gross (Chair of Arizona EMS Protocols, Medications, and Devices Committee) http://www.azdhs.gov/documents/preparedness/emergency-medical-services-trauma-system/advisory/MDC/PMDmembership.pdf 7. Bentley Bobrow (ADHS BEMS Medical Director and Chair of Arizona’s Medical Direction Commission) http://www.azdhs.gov/documents/preparedness/emergency-medical-services-trauma-system/advisory/MDC/MDCmembership.pdf 8. Eric West (Operations manager at Arizona Ambulance Association) http://www.azambulance.org/members/userprofile/abca139.html 9. Jerry Romero (President of Acadian Ambulance Services) https://www.acadianambulance.com/site870.php 10. Wendy Ord (Dispatch Manager and Safety Officer of Angel MedFlight) https://www.angelmedflight.com/air-ambulance-company.html 11. Kenny Rozenberg(CEO of Centers Health Care) http://centershealthcare.com/about/leadership 12. Michelle Robertson (CEO Seton Family of hospitals) https://www.seton.net/about-seton/seton-leadership-team/seton-family-of-hospitals-leadership/ 13. Julie Greaves (Regional Medical Director of Fort Bend County) http://www.fortbendcountytx.gov/index.aspx?page=440 http://www.dshs.texas.gov/region6-5/default.shtm 14. Keith Wages(Georgia State Office EMS Director) https://dph.georgia.gov/state-office-ems-directory 15. Donna Pattet (Director of Nursing at Advanced Health Care of Scottsdale) http://ahcfacilities.com/rehabilitation-facilities/scottsdale 16. Lorraine Lutton (President of St. Joseph’s Hospital) http://www.sjhfoundation.org/about/board-of-directors/ 17. Dr. Silvio D. Morales (Medical Director of Aerocare Air Ambulance Service) http://www.sjhfoundation.org/about/board-of-directors/ 18. Wade Spruill (CEO of AAA Ambulance Service) https://aaaambulance.net/leadership/ 19. Edward Van Horne (CEO of American Medical Response) https://www.amr.net/about/leadership 20. Dr. Kim Landry (Chief Medical Officer of Lifeguard Ambulance Service) https://www.lifeguardambulance.com/aboutus/leadership-team Competitors
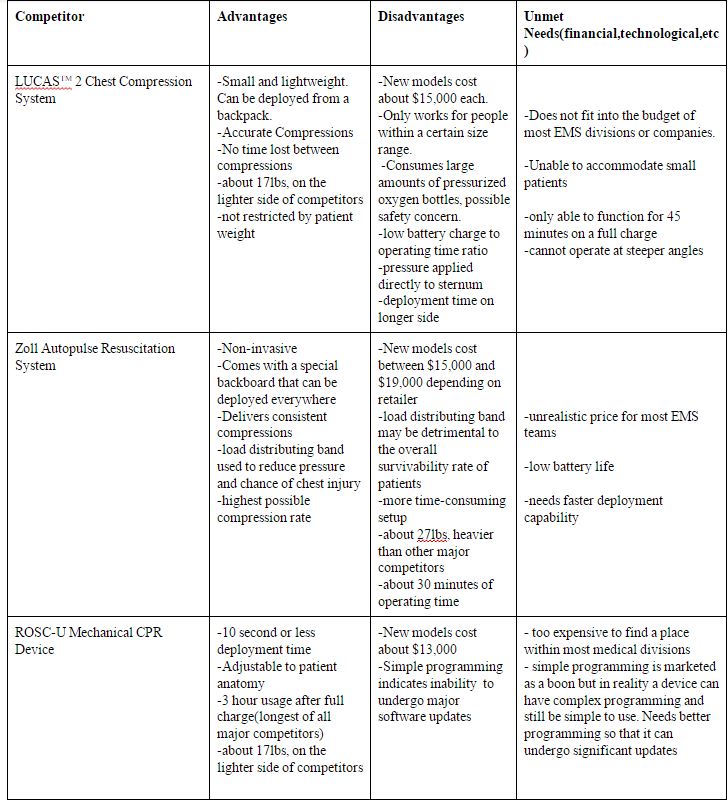
Zoll Autopulse: https://www.ncbi.nlm.nih.gov/pubmed/16772625?dopt=Abstract https://www.zoll.com/medical-products/resuscitation-system/autopulse/ems/ http://defibshop.com.au/shop/autopulse-non-invasive-cardiac-support-pump/
Defibtech Lifeline Arm: https://www.medicaldevicedepot.com/Defibtech-Lifeline-ARM-p/rfc-a1000en.htm
IP Position
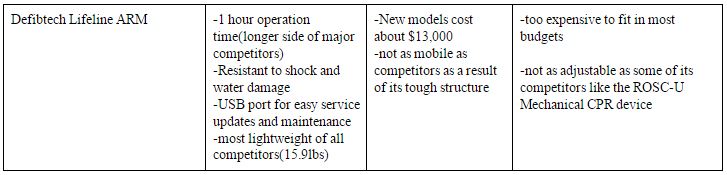
Mechanical Chest Compression Device with tilt sensor, US 20140046228A1, Robert G Walker, 07-25-2013, pending patent
Summary: Uses an external chest compressor which uses a piston to apply each compression. The external chest compressor is aided by belts or some other fastening mechanism which can help with securing the patient’s chest for pressure to be applied. The primary standout feature is a tilt detector that will take the form of a buzzer or light to inform either the medical officer or machine that the axis has tilted. This concept of a tilt sensor could be tweaked and applied to our proposed device by making it more of a level sensor when medical technicians are setting up our device on a surface like a stretcher.
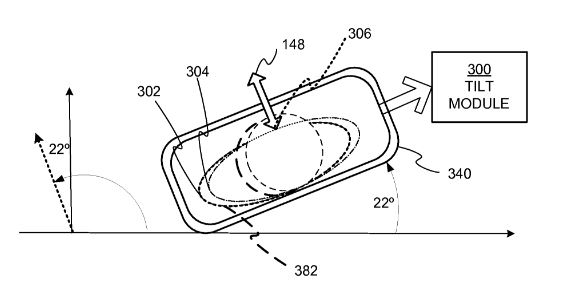
Light weight chest compressor, US 20050148909, Max Weil-Joe Bisera-Carlos Castillo, 02-08-2005, pending patent
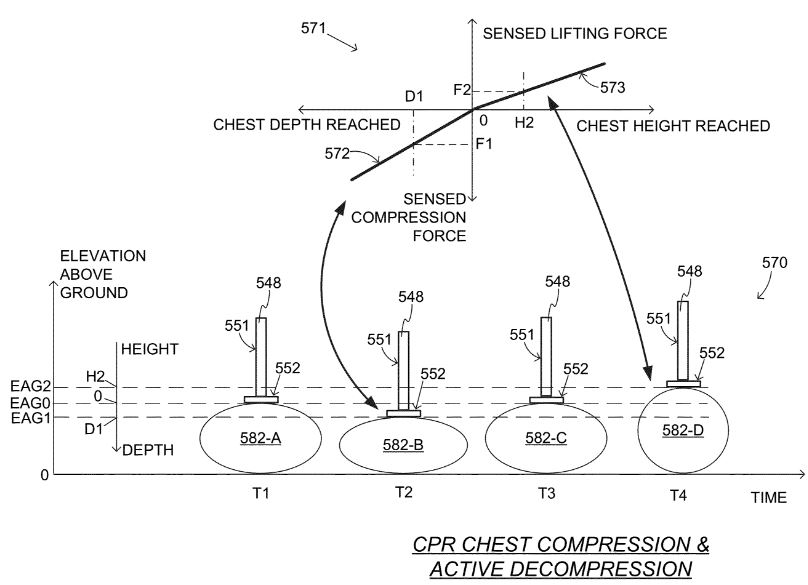
Summary: Utilizes a piston to apply compression force to a patient’s chest. Features a force sensing system in tandem with a driver system that allows the machine to create a motion-time profile. The motion-time profile allows the machine to adjust pressure or engage the built-in chest-lifting device if an unexpected amount of time elapses between each compression motion. This allows the machine to self adjust to outside disturbances. The ability for our device to be self-adjustable to a certain extent would be useful in successfully creating a device that is operable while being shaken around as EMS units traverse across terrain.
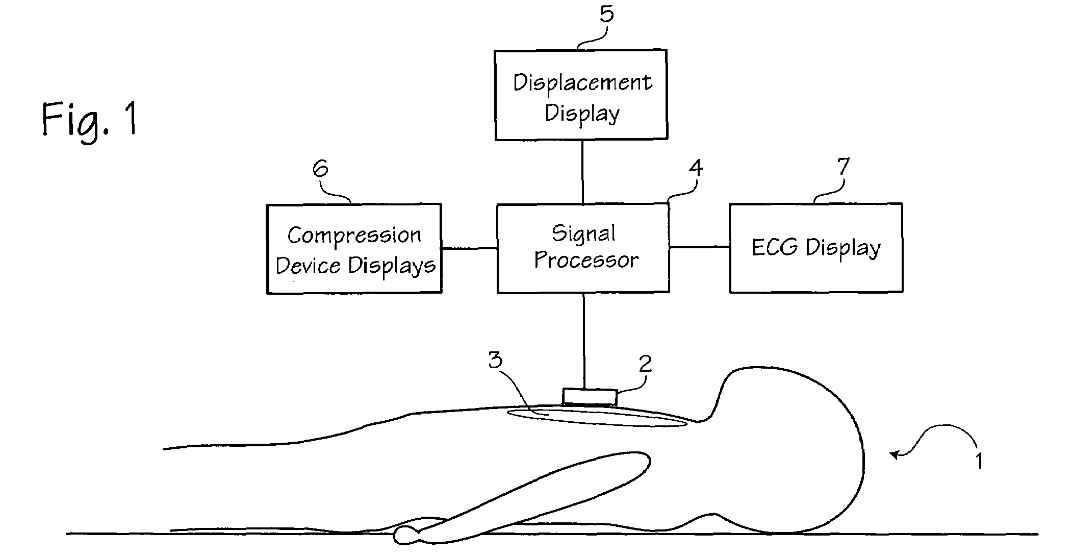
Summary: Although not necessarily originally developed for automated CPR devices, this technique employs the usage of accelerometers and reference sensors to achieve a measurement of compression depth. The assignee of this patent is Zoll, one of the major competitors in the ACCD market. They likely modified this technique in a way that it could be integrated into their ACCD. Our device will also need a mechanism to measure depth compression and while more modern methods are likely to be the most accurate, a modification of an earlier method could result in a cheaper measuring mechanism. Fundability Worksheet Scores
| |||||||