Artificial Trachea, by Ian Costello: Difference between revisions
No edit summary |
No edit summary |
||
| Line 20: | Line 20: | ||
== Tracheal Cancer == | == Tracheal Cancer == | ||
[[ | [[Image:tracheal_tumor.jpg|frame|thumb|right|400px|Tumor blocking air passage in trachea [7].]] | ||
The loss of normal airway function due to a tracheal tumor can quickly become lethal. The tumor may grow uninhibited until it is completely blocking airflow if untreated. Tracheal tumors are very rare. There are about 1,800 cases in the United States each year with about a five percent survival rate. One of the major problems with tracheal cancer is incorrect diagnosis because the symptoms are so similar to other medical conditions like asthma. Symptoms include coughing, wheezing, shortness of breath, and in later stages fatigue and difficulty breathing caused from a partially blocked windpipe. Tracheal tumors are a huge motivation for the development of artificial tracheas due to the fact that other treatments such as stenting and chemotherapy fail after a certain point [4] [5]. | The loss of normal airway function due to a tracheal tumor can quickly become lethal. The tumor may grow uninhibited until it is completely blocking airflow if untreated. Tracheal tumors are very rare. There are about 1,800 cases in the United States each year with about a five percent survival rate. One of the major problems with tracheal cancer is incorrect diagnosis because the symptoms are so similar to other medical conditions like asthma. Symptoms include coughing, wheezing, shortness of breath, and in later stages fatigue and difficulty breathing caused from a partially blocked windpipe. Tracheal tumors are a huge motivation for the development of artificial tracheas due to the fact that other treatments such as stenting and chemotherapy fail after a certain point [4] [5]. | ||
| Line 31: | Line 31: | ||
== Artificial Trachea == | == Artificial Trachea == | ||
[[ | [[Image:400px-procedure_2.png|frame|thumb|left|400px|Before, during, and after artificial trachea incubation [2].]] | ||
The artificial trachea is the largest organ grown completely in the laboratory without the aid of donor tissue. The scaffold for the artificial trachea is made from Poly-ethylene terephthalate (PET), a biodegradable plastic commonly found in water bottles. The scaffold is sized according to scans of the patients own trachea so it can be custom fitted. Once the artificial scaffold is made, it is seeded with stem cells in a similar way to the cadaver trachea. The benefit here is that the scaffold does not need to be chemically treated to remove cells as there never were cells on the scaffold. The scaffold is placed in a bioreactor designed by Harvard Bioscience Inc. where the stem cells and certain transcription factors are added. The scaffold incubates for two days and the stem cells attach to the scaffold and begin to differentiate. The artificial trachea is then transplanted into the patient. Some advantages the artificial trachea has over the donor trachea include being able to custom-fit the trachea to the patient, not needing a donor, and zero immunogenicity issues. The procedure costs roughly $450,000 [1] [2] [3]. | The artificial trachea is the largest organ grown completely in the laboratory without the aid of donor tissue. The scaffold for the artificial trachea is made from Poly-ethylene terephthalate (PET), a biodegradable plastic commonly found in water bottles. The scaffold is sized according to scans of the patients own trachea so it can be custom fitted. Once the artificial scaffold is made, it is seeded with stem cells in a similar way to the cadaver trachea. The benefit here is that the scaffold does not need to be chemically treated to remove cells as there never were cells on the scaffold. The scaffold is placed in a bioreactor designed by Harvard Bioscience Inc. where the stem cells and certain transcription factors are added. The scaffold incubates for two days and the stem cells attach to the scaffold and begin to differentiate. The artificial trachea is then transplanted into the patient. Some advantages the artificial trachea has over the donor trachea include being able to custom-fit the trachea to the patient, not needing a donor, and zero immunogenicity issues. The procedure costs roughly $450,000 [1] [2] [3]. | ||
Revision as of 02:56, 31 July 2012
Background
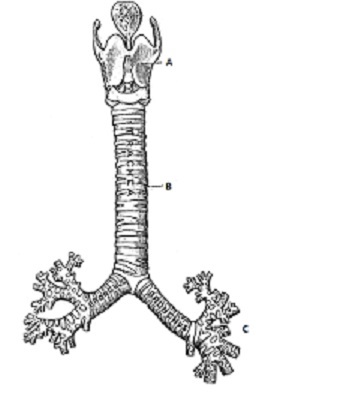
The trachea (also known as the windpipe) is composed of cartilage, muscular fibers, a mucous membrane, and various glands. The trachea, roughly 11 cm long in an adult, connects the larynx to the left and right bronchus and its main role is as an air passageway. It is lined with epithelial cells which produce a mucus membrane that is essential to several important tracheal functions. This mucus is responsible for catching dust and bacteria before the air reaches the lungs and this unwanted material is expelled from the body as phlegm (via coughing or sneezing). This mucus also moistens the air before it enters the lungs [5].
Trachea Conditions
The loss or of proper functioning in the trachea from tracheal cancer, tracheomalacia, or any other reason can be devastating to normal airflow in the windpipe [5].
-Tracheoesophageal fistula: This is when a channel forms between your esophagus and trachea. The esophagus is responsible for transport of food and water. When a channel forms between the esophagus and trachea, food and water may travel down the windpipe possibly causing damage to the lungs [5].
-Tracheomalacia: This is when the trachea is soft, flaccid, or floppy instead of rigid. This is usually due to a birth defect but smoking or various injuries may cause this as well [5].
-Tracheal stenosis: This is scarring or inflammation of the trachea which may lead to a narrowing of the passageway. If severe enough, surgery or a tracheal stent may be required to treat this condition [5].
-Tracheal Cancer: Although very rare, when this occurs a tumor may grow in the trachea to a point where it’s blocking airflow [5].
Tracheal Cancer
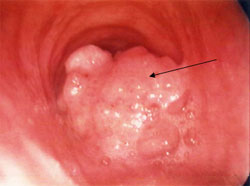
The loss of normal airway function due to a tracheal tumor can quickly become lethal. The tumor may grow uninhibited until it is completely blocking airflow if untreated. Tracheal tumors are very rare. There are about 1,800 cases in the United States each year with about a five percent survival rate. One of the major problems with tracheal cancer is incorrect diagnosis because the symptoms are so similar to other medical conditions like asthma. Symptoms include coughing, wheezing, shortness of breath, and in later stages fatigue and difficulty breathing caused from a partially blocked windpipe. Tracheal tumors are a huge motivation for the development of artificial tracheas due to the fact that other treatments such as stenting and chemotherapy fail after a certain point [4] [5].
Trachea Transplant (from cadaver)
Since 2008, there have been 10 trachea implants using tracheas from cadavers. The tracheas are harvested and chemically treated to remove all original cells. Once the cells have been removed from the donor trachea, it is essentially used as a scaffold. Stem cells are taken from the patient’s bone marrow and are seeded onto the scaffold trachea. The scaffold is inserted into a bioreactor where the patients stem cells and certain transcription factors are added to induce specific differentiation on the scaffold. Once the cells have differentiated to a certain point, the trachea is implanted into the patient where the body takes over and induces more cell differentiation and proliferation. There are a few issues with this type of transplant. Donor tracheas are not in high supply and even then the donor tissue may not be a good fit for the patient with regards to size. As with any donor tissue there is always a chance that immunogenicity problems may arise as well [6].
Artificial Trachea
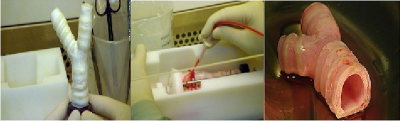
The artificial trachea is the largest organ grown completely in the laboratory without the aid of donor tissue. The scaffold for the artificial trachea is made from Poly-ethylene terephthalate (PET), a biodegradable plastic commonly found in water bottles. The scaffold is sized according to scans of the patients own trachea so it can be custom fitted. Once the artificial scaffold is made, it is seeded with stem cells in a similar way to the cadaver trachea. The benefit here is that the scaffold does not need to be chemically treated to remove cells as there never were cells on the scaffold. The scaffold is placed in a bioreactor designed by Harvard Bioscience Inc. where the stem cells and certain transcription factors are added. The scaffold incubates for two days and the stem cells attach to the scaffold and begin to differentiate. The artificial trachea is then transplanted into the patient. Some advantages the artificial trachea has over the donor trachea include being able to custom-fit the trachea to the patient, not needing a donor, and zero immunogenicity issues. The procedure costs roughly $450,000 [1] [2] [3].
Results
There have been two patiens thus far that have received the artificial trachea. The first artificial trachea was implanted in June 2011 by Paolo Macchiarini, M.D., Ph.D. There have not been immunogenic issues and the patients to do not take anti-rejection drugs. Andemariam Teklesenbet was the first patient to receive the artificial trachea and so far the trachea is showing great results as he is breathing, talking, and coughing without difficulty. The second patient to receive the artificial trachea has since deceased. It is too early to determine how viable the procedure is going to be as there isn’t any significant statistical data yet but more work is being done to make this a practical option for treatment [3].
References
[1] Fountain, Henry. "Synthetic Windpipe Is Used to Replace Cancerous One." New York TImes. 12 Jan. 2012. Web. 10 Apr. 2012. <http://www.nytimes.com/2012/01/13/health/research/surgeons-transplant-synthetic-trachea-in-baltimore-man.html?_r=4>.
[2] "In Medical First Doctors Implant Lab Grown Synthetic Trachea Into Patient." Singularityhub. Web. 13 Apr. 2012. <http://singularityhub.com/2011/07/09/in-medical-first-doctors-implant-lab-grown-synthetic-trachea-into-patient/>.
[3] Sternberg, Steve. "Patient Gets World's First Artificial Trachea." USA Today. Gannett, 08 July 2011. Web. 13 Apr. 2012. <http://www.usatoday.com/news/health/story/health/story/2011/07/Patient-gets-worlds-first-artificial-trachea/49176868/1>.
[4] "Tracheal Cancer." Macmillan.org. Dec. 2011. Web. 12 Apr. 2012. <http://www.macmillan.org.uk/Cancerinformation/Cancertypes/Tracheawindpipe/Trachealcancer.aspx>.
[5] "The Trachea (Human Anatomy): Picture, Function, Conditions, and More." WebMD. WebMD, Sept. 2009. Web. 13 Apr. 2012. <http://www.webmd.com/lung/picture-of-the-trachea>.
[6] "Cancer Patient Pioneers First Stem Cell Trachea Transplant - HSCC Online Provide News Spotlight about Stem Cell and Medicine - HSCC Online Provide News Spotlight about Stem Cell and Medicine." Hongkong Stem Cell Centre -Hong Kong Stem Cell Centre, Jan. 2012. Web. 12 Apr. 2012. <http://www.hongkongstemcell.com/c/e_information_244.php>.
[7] "NYU Voice Center - Tracheal Tumor." Med.nyu. NYU, 2005. Web. 13 Apr. 2012. <http://www.med.nyu.edu/voicecenter/resources/photo/tracheal_tumor.html>.
[8] "Trachea Clipart." Educational Technology Clearinghouse. Web. 13 Apr. 2012. <http://etc.usf.edu/clipart/15400/15499/trachea_15499.htm>.