840.119:Xenotransplantation
Xenotransplantation: The production of porcine organs for use in humans.
State of the Art
By definition, xenotransplantation is: the surgical transfer of cells, tissues, or especially whole organs from one species to another.
Xenotransplantation consists of scientists searching for methods to produce in animals organs suitable for transplant into people. Unfortunately the waiting list for heart transplants keeps getting longer and longer. A new source of hearts and other organs could save or improve the lives of thousands of people waiting for tlimited supply of available human organs. Yes, if we had an increase in willing organ donors the need for porcine parts, or xenotransplantation would decrease, and when looking at alternatives pigs appear to be the best choice. This is because the pig is compatible in size and physiology of humans.
Although xenotransplantation has been around for over hundreds of years, successes have been few and far between. The use of pig organs began approximately ten to fifteen years ago. One common procedure is the transplanting of pig heart valves into humans. In an imagined world, xenotransplantation is quite simple. If a patient showed signs of organ failure, the failing organ could be replaced with a suitable pig organ. Xenotransplantation would in turn minimize suffering and physical deterioration if early action is taken. Patients would'nt have to suffer from the depressing experience waiting for a donor organ, wondering if they will be dead before one becomes available. Some scientists believe it may take five to seven years before whole organ xenotransplantation of pigs-to-humans becomes reality. According to David Ayares, chief opperating officer and vice president of research at PPL, "We're now ready to go into pivotal pig-to-primate trials and needs to show in excess 90-day survival before regulatory authorities approve human trials".
Beacause the size of pig organs is similar to that of humans, they are considred one of the best sources for transgenic transplants. If your asking why not a primate as a organ donor instead of the pig, being that the chimpanzee is the primate most appropriate to serve as a donor. Because they share more than ninety-eight percent of their genes with humans. But chimp's are an endangered species and dont breed as well as pigs. Pigs are easily bred at fast rates and in large numbers. The quality of the pig organs in xenotransplantation is also higher, they dont have to be severed from the blood supply and kept functioning until the transplant takes place, which reduces the tissue damage. The pig organs are also healthier because they are bred, fed, and protected from disease with focus on producing organs that are as perfect as possible. Human donor organs have the possibility of coming from unhealthy people. The pigs are genetically modified or have certain genes turned off to over come rejection issues in humans.
Xenotransplantation is important because every day more people are added to the waiting list for ogans. Clinical transplantation has become one of the preferred treatments for end-stage organ failure since the introduction of chronic immunosuppressive drugs in the mid-1980's. Xenotransplantation is one of the novel approaches to dealing with the limited supply of human organs. Over sixty percent of people on the list die before they can recieve an organ. In one study, out of 140 patients referred for heart transplants only about twenty-five recieved the heart they desperately needed. It is estimated that out of the eighty-thousand people who need a transplant each year, only twenty-four thousand recieve an organ. Sadly, many people die while they are still waiting.
Objectives
The focus of this page is to explain the scientific approach being taken to achieve sucessful pig to human organ transplantation.
Scientific Approach
The technique is progressing at a fairly rapid pace. There have been successful transplants from pigs to sheep. The next step is transplanting from pigs to baboons, which are much more closely related to humans.
Unaltered porcine organs transplanted into other mammals do not last very long. In the article "Xenotransplant" it was said that "Without extremely high levels of immunosuppressive drugs, pig organs seldom last half an hour." By bioengineering pigs to lack certain genes or replace them with human genes it is possible to greatly increase the life of the organ after transplantation. This has been proven in research where the gene for a certain sugar enzyme was deleted from the pig. The hearts of the pigs were then placed in the abdomens of eight baboons. Of these eight baboons five lived between 2-6 months with the aid of immunosuppressants.
There is a sugar protein, a 1,3 galactosyl epitope (determining factor), which triggers immune-system rejection in transplants to humans. Progress has been made to overcome this problem by genetically modifying the pigs and inactivating these genes. Once a genetic change is made in the population, these new "donor animals" can be bred easily by conventional techniques. The major barrier to progress in pig-to-human organ transplants is the presence of the terminal 1,3 (GAL) epitopes on the surface of pig cells. Humans have lost the corresponding GAL activity in the course of evolution and therefore produce performed natural antibodies to the epitope.
Some companies used cloning techniques to produce piglets with organs more likely to be accepted by humans in a transplant operation. The genetically modified pigs lacked one of the two copies of a gene that makes a sugar called alpha-1,3 galactose, the substance that triggers the immune system rejection in transplants to humans. Tissues from these pigs are "completely devoid" of the pig sugar that spurs the rejection. Scientist took skin cells from a pig fetus that already had one copy of the relevant genes knocked out and deactivated the second copy of the gene in the cells.
This pig heart is being infused with blood plasma containing antibodies from a sheep to help it resist rejection when it is implanted into a sheep. (PHOTO COURTESY UNIVERSITY OF NEBRASKA MEDICAL CENTER)
Tissue engineering is another possible alternative to xenotransplantation. If tissue engineering becomes successful it will dynamically change the field of organ transplantation. Tissue engineering is the process of creating functional tissues using cells combined with devices that facilitate cell growth. Tissue engineering has several applications as a substitutive therapy for organ transplantation. The first generation of tissue engineering is the creation of immunoisolated devices that combine living cells and biomaterials. This technique uses hydrogel membranes as a barrier of the foreign living cells from the lymphocytes of the immunocompatent host.
This approach has very realistic possibilieties for medical devices and treatment. The future of tissue engineering products is with the research of stem cells and therapeutic cloning. The technology of harvesting embryonic stem cells from the inner cell mass of blastocysts introduces the potential to procuce any thype of cell using the appropriate needs for differentiation. This technique would make it possible for biologists to grow any functional tissue or organ. The need for immunosuppression for this technique would be eliminated through therapeutic cloning. This is a process where stem cells are used to tissue engineer organs for transplantation. The organs would be inherently "self" organs, with self-antigens. The immune system would have no incentive to attack the new organ. There are some drawbacks to this therapy which include manufacturing problems. This is because each organ must be created specifically for each individual. There would be a time space between identification of the need for a transplant and production of a fully functional organ. Other problems include the ethical issues surrounding stem-cell research. Controversy with this issue isn't suprising, considering that many stem-cell issues parallel the issues with abortion. Currently, human embryonic stem cells are heavily regulated by the government and viewed by many as ethically repulsive.
Pre-clinical studies on adult stem cell based therapies have been inconsistent, with alot of them resulting in contradicting outcomes. Results of several allegedly successful studies cannot be repeated reliably. As an example, one study's use of marrow-derived adult stem cells to regenrate a significant amount of necrotic tissue in an infarcted cardiac zone was questioned when other groups were unable to duplicate results. Despite problems, tissue engineering is in fact a developing therapy.
Impact (Potential)
Because there are too many people in need of organ transplants and not enough organs being donated, thousand die each year while they wait. The table below shows the number of people on the National Transplant Waiting List waiting for a specific organ. Using the liver for an example, there are there are 7,551 women waiting for a liver and 10,356 men, just in this country, and just for a liver.
Table 1. Number of Individuals on the National Transplant Waiting List as of May 2001
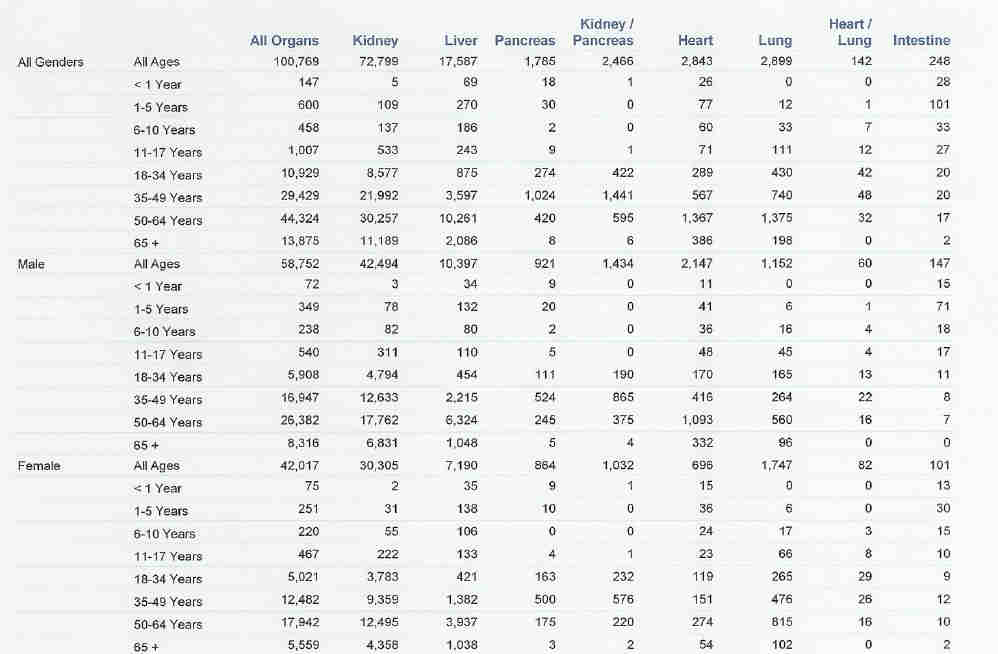
If we were able to take the organs from another animal, in this case the pig, to transplant into humans successfully we may be able to overcome the deficit and save thousands of lives. In addition, with genetic engineering we may be able to make these organs better for transplanting than human organs. The organs may last longer than those transplanted from humans as well as perform better. While we are unable to manipulate the human genome it is possible to do experiments with animals that can be applied to humans.
Associated Risks
There are several risks associated with pig to human transplantations. There are some diseases that can be transferred from pigs to humans. Pigs have a very promising future due to their tissues being relatively free of potentially toxic agents. While many diseases are species specific there are some that can be transferred. One specific example is porcine endogenous retrovirus, which is produced by the pig pancreatic islet cells. Porcine endogenous retrovirus is dormant in pigs. Doctors feel, however, it is possible that transplanting the organs into humans could reactivate the virus. It has been shown in laboratory conditions that the virus can be transferred from pig to human tissues. There is also a fear that xenotransplants may make it easier for viruses to cross the species barrier.
Other risks include the possibility of rejection. There are galactose α-1,3-galactose residues on the surface of pig cells that are not present in humans. Because the human immune system doesn’t recognize these residues they will try to destroy the pig cells. The picture shown below is of aortic endothelial cell activation in a pig-primate model of xenographt rejection.
Another major concern is the possiblilty that animal virus residing in a xenograft recipient may become airborn. Because we don’t have antigens against this virus (there is no human equivalent) thousands of people might die before a vaccination could be created.
Ethical Issues
There is much controversy about using pig organs for transplant. Some people feel that we don’t have a right to kill other animals just to aid our own ends. A specific example is PETA, a very outspoken animal rights group.
Others feel that by putting the organs of a different species of animal into our bodies we will be losing some of our humanity. Individuals view their internal bodies as an extension of their identities, and soon after the xenotransplantation, some patients will realize the consequences of their actions on their self-concepts. Having an animal's organ in one's body has the potential to decrease our self-image despite intense counseling on the neutrality of this occurrence.
Some people view xenotransplantation as an involuntary form of human experimentation violating US laws and UN charters. We can’t know the exact effects the organ will have until it is transplanted. And because it may cause diseases to cross the species barrier, people may unwillingly be subjected to new diseases that they wouldn’t otherwise contract.
Xenotransplatation is more expensive than human-to-human transplantation (roughly $300,000 per operation, not including the hidden costs of breeding, housing, feeding, medicating, testing, transporting, rendering, and disposing of the waste and remains of herds of transgenic animals) making it unaffordable for most people. While some people are trying to make life better for us, there are others who’s only goal is making money. Companies may develop monopolies over artificially engineered and created species, allowing them to charge even more for the organs. As the process is refined these costs will hopefully decrease.
Currently, the wealthy and powerful get first access to transplants. We need to allocate organs as per top priorities. There is hope that using pig organs we will be able to change this, letting those who need a transplant the most recieve an organ first.
References
Baker, Monya. "Xenotransplant". Technology Review. 108 (5) 2005. 86.
http://education.guardian.co.uk/higher/biologicalscience/story/0,,627038,00.html
http://www.uq.edu.au/oppe/PDFS/Xenotransplantation.pdf
Lai, Liangxue. "Production of α-1,3-Galactosyltransferase Knockout Pigs by Nuclear Transfer Cloning". Science. 295 (5557) 2002. 1089.
Naik, Gautam. "Health and Technology: Cloned Piglets May Aid Organ Hunt---PPL Therapeutics Makes Gain in Effort to Improve Translants' Success Rate". The Wall Street Journal. New York, N.Y.: Aug 23, 2002. pg A8.
Winslow, Ron. "Scientists Clone Pigs, Lifting Prospects of Replacement Organs for Humans". The Wall Street Journal. New York, N.Y.: Aug 17 2000. pg A6.
http://net.unl.edu/newsFeat/med_eth/me_xeno.html
http://www.crt-online.org/wrong.html
http://www.technologyreview.com/read_article.aspx?id=17596&ch=biotech
http://dictionary.reference.com/browse/xenotransplantation
http://www.optn.org/latestData/rptData.asp
Munson, Ronald. "Raising The Dead: Organ Transplants, Ethics, and Society". Oxford, New York.: 2002. Pages 192-220.
http://biomed.brown.edu/Courses/Bi108/BI108_2004_Groups04/Tissue_Engineering.htm